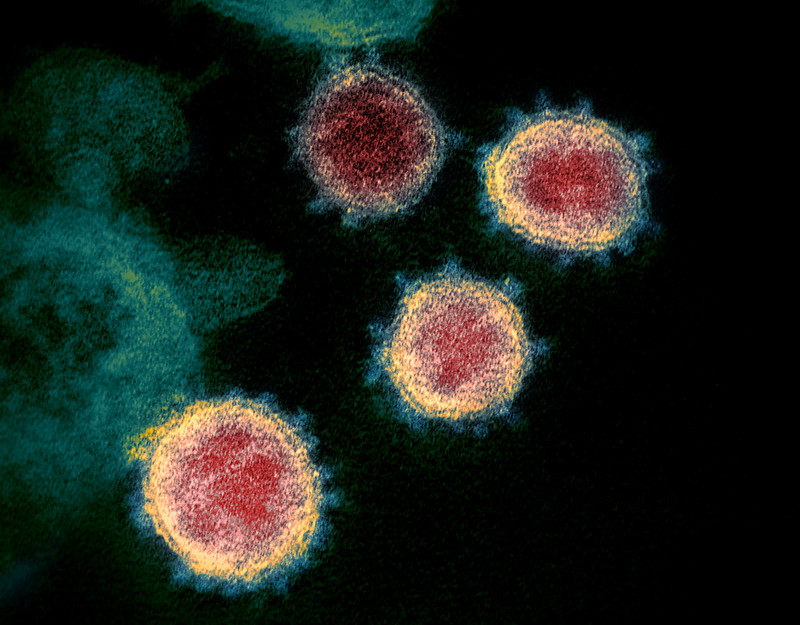
Getting COVID-19 multiple times dramatically increases the risk of developing long COVID. Research from Stony Brook University shows 85% of long COVID patients had repeated infections. “Having COVID numerous times makes patients more at-risk,” says Dr. Sean Clouston, explaining how this condition can persist long after the initial infection clears.
Long COVID is defined by the CDC as a chronic condition that occurs after COVID-19 infection and is present for at least three months. The symptoms can range from mild to severe, affecting different parts of the body. Many patients find basic daily activities become challenging.
Nenia Ballard knows this firsthand. Once a police officer and CrossFit athlete, she now uses a wheelchair. “I pulled up to an intersection and didn’t know where I was,” she recalls about the brain fog that forced her to leave her job. “That was how I kept myself safe and alive. I had to be able to think quickly.”
The numbers tell a troubling story. In New Hampshire, 4,000 people had to quit working because of the long COVID. Another 5,300 cut back their hours. Dr. Jeffrey Parsonnet at Dartmouth’s Post Acute Covid Syndrome Clinic has seen 800 patients struggling with these lasting effects.
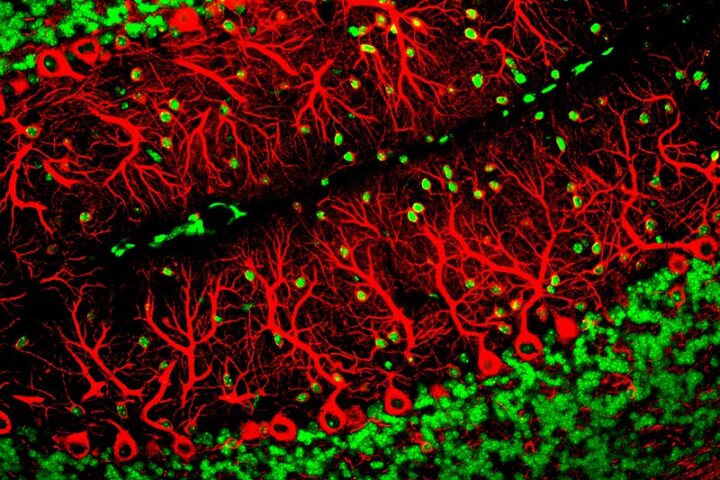
Dr. Parsonnet explains that long COVID is “really a different illness” from COVID-19. While COVID-19 is respiratory, long COVID is neurologic. About 68% of patients still feel tired, confused, or short of breath two years later. Having high blood pressure, severe COVID, or no vaccination makes it more likely.
“Most working-age patients didn’t recover in the second year,” report German researchers who studied 982 adults. They found exercise especially hard – 35% couldn’t handle physical activity without getting worse. According to the CDC, symptoms typically worsen 12 to 48 hours after activity.
State Representative Wendy Thomas has lived with long COVID since 2020. She lost her sense of taste and smell, dropped 85 pounds, and faces ongoing health challenges. “This impacts our economy,” she warns. “People end up on disability when they could be working.”
Similar Posts
The cost goes beyond money. Kate Harmon Siberine, a former priest, spends 85% of her time in bed now. “I never could’ve anticipated being here three years later with the same symptoms,” she shares. Her medical team told her to stop working or risk getting worse.
Dr. Christina Martin, who treats long COVID patients, admits there’s still much to learn. “We’re willing to guess, but we’ll tell you it’s just a guess,” she says about predicting recovery. This uncertainty affects how patients plan their futures, from work choices to living arrangements.
The Post Acute Covid Syndrome Clinic focuses on managing symptoms while research continues to understand this condition. Medical teams work with patients to help them adapt to their current limitations while looking for effective treatments.