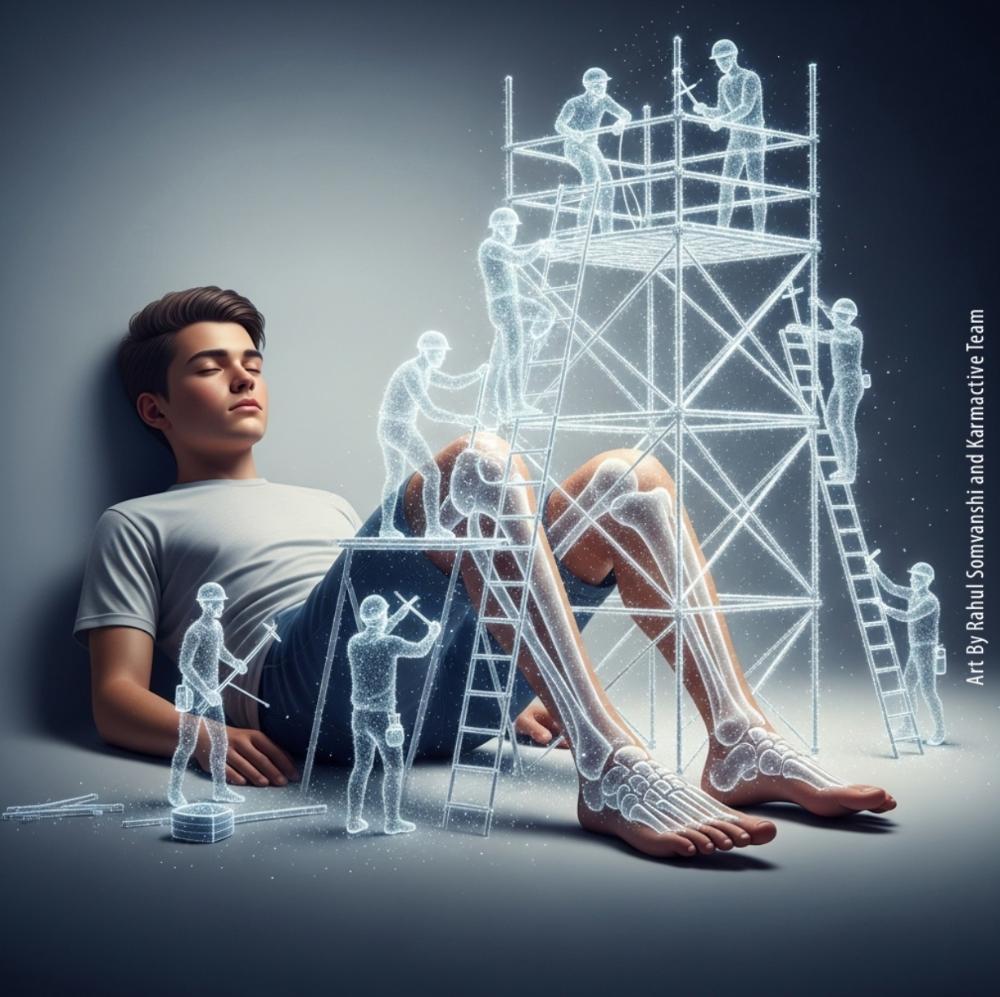
Teenage years build the skeletal foundation for life, but new research reveals that obesity and type 2 diabetes can sabotage this crucial process. A study presented at ENDO 2025 found that teens with obesity and type 2 diabetes showed less improvement in bone strength and quality over time compared to their normal-weight peers.
The Study That Changes Everything
Dr. Fida Bacha from Baylor College of Medicine in Houston tracked 48 teenagers for one year, including 26 girls with an average age of 15.5 years. The research team divided participants into three groups: 27% had normal weight, 31% were overweight with normal blood sugar, and 42% had overweight with impaired blood sugar control, including 4 teens with prediabetes and 16 with type 2 diabetes.
Using high-resolution imaging, researchers measured bone structure and strength in the lower leg (tibia) and forearm (radius). They also tracked body fat, fitness levels, blood sugar, and insulin concentrations. The results were stark.
Teens with obesity, especially those with type 2 diabetes, showed less improvement in bone strength and quality during the study period. This pattern appeared in both leg and arm bones. Even more concerning, higher insulin levels – a hallmark of insulin resistance – contributed to reduced bone strength gains.
“We wanted to understand how childhood obesity and early type 2 diabetes affect bone health as children grow,” Bacha explained. The findings were troubling, particularly given the tiny brain cell cluster found to drive obesity and overeating that researchers have recently identified.
Why Teen Years Matter Most
Peak bone mass is likely achieved by late adolescence, representing the “bone bank” individuals draw from for their entire adult life. This window is incredibly narrow and powerful. Research shows that adolescents accumulate substantial bone mass during the years surrounding peak bone growth velocity.
The Saskatchewan Bone Mineral Accrual Study found that maximal peak bone mineral content velocity occurs at 14.0 ± 1.0 years in boys and 12.5 ± 0.9 years in girls. During the 2 years of peak skeletal growth, adolescents accumulate over 25% of adult bone mass.
About 95% of a young woman’s peak bone mass is present by age 20, with some gains continuing until age 30. This critical timing makes adolescence the most important period for building lifelong skeletal strength.
The Insulin Resistance Connection
Insulin resistance occurs when the body’s cells don’t respond effectively to insulin, leading to elevated blood sugar levels and increasing type 2 diabetes risk. This metabolic dysfunction creates a cascade of bone-damaging effects.
Previous research found that in youth with type 2 diabetes and obesity, bone mineral density was about 0.5 standard deviations lower compared to healthy-weight peers. The study also revealed that greater visceral fat was associated with lower bone density.
However, the relationship between diabetes and bone health is complex. While type 2 diabetes patients typically show increased bone density, this is misleadingly protective. The bones are denser yet more brittle due to microarchitectural defects, elevated fracture risk, and compromised bone quality from advanced glycation end products and inflammatory processes.
The Growing Crisis
The statistics paint a concerning picture. Type 2 diabetes prevalence among U.S. youth in 2017 was 0.67 cases per 1,000, corresponding to 1,230 cases among 1,848,899 youth aged 10-19 years. But the burden isn’t equally distributed.
The highest prevalence rates per 1,000 youth in 2017 were observed among Black or African American youth at 1.80, followed by 1.63 in American Indian youth, 1.03 among Hispanic youth, 0.59 among Asian/Pacific Islander youth, and 0.20 among non-Hispanic White youth.
From 2002 to 2012, the rate of new type 2 diabetes cases increased by 4.8% annually – faster than the 1.8% increase for type 1 diabetes. This rising trend contributes to what experts project as India’s obesity crisis affecting 440 million by 2050, with similar patterns emerging globally.
Similar Posts
Clinical Implications and Bone Quality
Youth-onset type 2 diabetes is characterized by rapid declines in pancreatic β-cell function and insulin resistance. Research suggests that the influence of type 2 diabetes on bone development depends on age, with the greatest effects evident at later developmental stages.
Type 2 diabetes accounts for one in three new childhood diabetes cases, with rising incidence among American Indian/Alaska Native, Black, and Hispanic/Latino children. This metabolic disorder creates a perfect storm for compromised bone health.The mechanisms behind diabetic bone disease include hyperglycemia, insulin resistance, and proinflammatory cytokines that disrupt normal bone turnover by affecting osteoblast and osteoclast function. Additionally, maternal obesity can reprogram fetal liver cells, with 60% of offspring developing fatty liver despite healthy diets, highlighting how metabolic dysfunction can begin before birth.
Treatment Considerations
“Obesity and early type 2 diabetes in adolescence don’t just affect weight or blood sugar—they can quietly interfere with bone development during the most critical years for building lifelong bone strength,” Bacha warned. “That means teens with these health issues may face a greater risk of fractures and osteoporosis as they get older.”
Recent therapeutic advances offer hope. GLP-1 drugs have been shown to cut obesity-linked cancer risk by 41%, surpassing surgical interventions. However, weight loss with Ozempic and Wegovy is often reversed post-treatment, emphasizing the need for long-term lifestyle interventions.
The accessibility of these treatments remains a concern, as evidenced by the Ozempic weight-loss craze hitting India’s gray market, where celebrities drive demand despite serious health risk concerns.
Understanding the Mechanism
Clinical studies in children and adults report that insulin resistance shows complex relationships with bone density, with both protective and harmful effects depending on severity levels. Advanced bone imaging methods now allow assessment of bone quality characteristics beyond standard bone mineral density measurements.
Lifestyle choices influence 20-40% of adult peak bone mass, making optimization of lifestyle factors crucial for reducing osteoporosis risk later in life. During puberty, half of total body calcium stores in women and up to two-thirds in men are accumulated.
The concept of a “Bone Bank” suggests that early deposits during youth lay the foundation for skeletal health, while later withdrawals during aging or metabolic stress can compromise skeletal integrity. This makes the teenage years particularly critical for interventions.
What Next
The research contributes to growing understanding of how metabolic health during adolescence shapes lifelong bone strength. Dr. Bacha’s study utilized established methodologies to track bone changes over time, providing concrete evidence of compromised skeletal development in teens with obesity and diabetes.
The study examined how these conditions affect the tibia and radius bones using precise imaging techniques, revealing measurable differences in bone development between healthy
teens and those with metabolic disorders. This work extends previous research on diabetic bone disease and insulin resistance effects on skeletal development.
For healthcare providers, these findings emphasize the importance of early detection and comprehensive management of obesity and diabetes in teenagers. The critical window for bone development during adolescence makes timely intervention essential for preventing long-term skeletal complications.
The research presented at ENDO 2025 provides valuable data on this critical health issue, offering new insights into the intersection of metabolic health and skeletal development during the crucial teenage years.