Hundreds of people taking popular weight loss and diabetes injections have reported serious pancreas problems, prompting UK health officials to launch a new study. The Medicines and Healthcare products Regulatory Agency (MHRA) is investigating an increase in reports of acute pancreatitis linked to GLP-1 medicines like Mounjaro, Wegovy, and Ozempic.
According to MHRA data, there have been nearly 400 reports of acute pancreatitis from patients using these medications, with 181 cases involving Mounjaro (tirzepatide). Since the beginning of 2025 alone, 101 pancreatitis cases have been linked to Mounjaro and 22 cases to Ozempic and Wegovy (semaglutide). Some cases have been fatal, with five deaths reported among Mounjaro users and one death each linked to other GLP-1 drugs.
“Alongside increased usage, we are seeing an upturn in the number of Yellow Card reports mentioning GLP-1 medicines and acute pancreatitis,” an MHRA spokesperson said.
What is Pancreatitis?
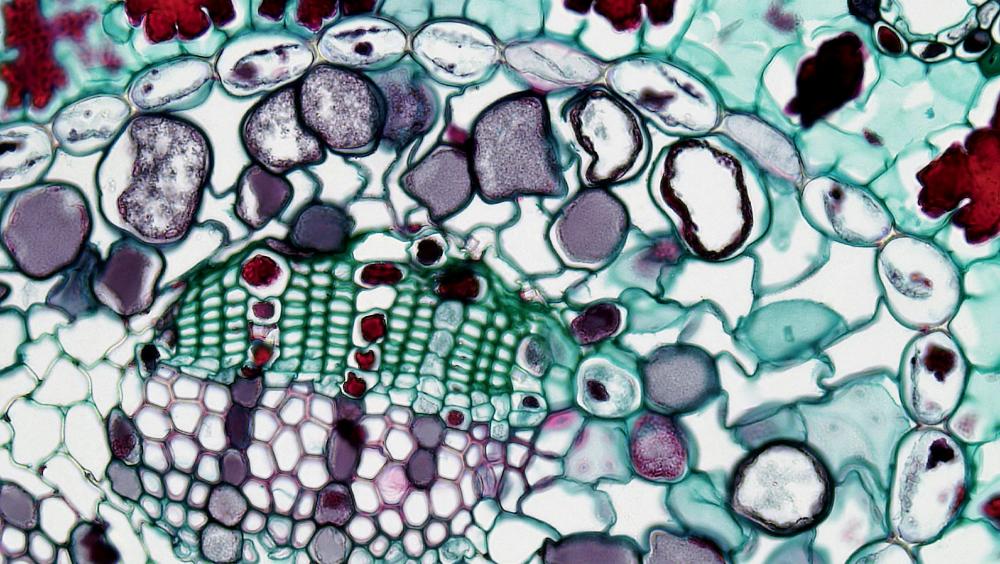
Acute pancreatitis is a sudden inflammation of the pancreas, an organ behind the stomach that helps with digestion and produces insulin. The condition often requires hospitalization and causes symptoms including severe abdominal pain, nausea, vomiting, and fever. While most patients recover within days, complications can occur, and about 5% of acute cases are fatal.
How Do These Drugs Affect the Pancreas?
GLP-1 drugs work by mimicking a naturally occurring hormone that stimulates the pancreas to produce insulin. In some cases, this increased stimulation might trigger inflammation in the pancreas. The risk appears to be higher in people with existing risk factors for pancreatitis, such as high triglyceride levels or a history of pancreas problems.
Dr. Rekha Kumar, an associate professor of medicine at Cornell, explains the mechanism: “The reason GLP-1 receptor agonists can cause pancreatitis is because the medications stimulate the pancreas to make insulin, so in an already inflamed organ, this might tip someone over the edge.”
Some research suggests that pancreatitis might also develop as a secondary effect of rapid weight loss, which can lead to gallstone formation – a known cause of pancreatitis. This could explain why some cases occur after months of treatment rather than immediately.
Who’s Most at Risk?
Recent research presented at the American College of Gastroenterology found several factors that might increase pancreatitis risk with GLP-1 drugs:
- History of type 2 diabetes
- Tobacco use
- Advanced chronic kidney disease
Interestingly, having a higher BMI (over 36) appeared to be protective against developing pancreatitis in some studies.
Similar Posts
Real Patient Experience
Julie Bishop, 55, shared her experience after being diagnosed with acute pancreatitis while taking Mounjaro. “I suddenly got a severe pain around my stomach and when it became clear I couldn’t walk it off, I went to the local walk-in centre,” she told The Independent. After blood tests at the hospital, she was diagnosed with pancreatitis and told to stop taking Mounjaro.
Bishop had lost two-and-a-half stone in eight weeks on the medication before her diagnosis. She has since suffered additional pancreatic “attacks” requiring hospital treatment.
What’s Being Done?
The MHRA is collaborating with Genomics England on the Yellow Card Biobank project to investigate whether genetic factors influence the risk of developing pancreatitis while taking these medications. Patients hospitalized with suspected drug-related pancreatitis are being encouraged to provide saliva samples for genetic analysis.
“Evidence shows that almost a third of side-effects to medicines could be prevented with the introduction of genetic testing,” said Dr. Alison Cave, the MHRA’s chief safety officer.
What Do Drug Manufacturers Say?
Manufacturers of these medications note that patient information leaflets already list pancreatitis as an “uncommon” side effect, potentially affecting up to 1 in 100 people.
A spokesperson for Lilly, which makes Mounjaro, stated: “Patient safety is Lilly’s top priority. We take reports regarding patient safety seriously and actively monitor, evaluate and report safety information for all our medicines.”
Similarly, Novo Nordisk, maker of Ozempic and Wegovy, emphasized that patients should take these medications only for approved uses and under healthcare supervision.

What Should Patients Do?
Healthcare professionals advise:
- Only take these medications under proper medical supervision
- Discuss any history of pancreatitis with your doctor before starting treatment
- Be aware of pancreatitis symptoms: severe abdominal pain (often radiating to the back), nausea, vomiting, and fever
- Seek immediate medical attention if these symptoms develop
- Report any suspected side effects to the MHRA’s Yellow Card scheme
While these reports are concerning, experts note that for many people with type 2 diabetes or obesity, the benefits of GLP-1 drugs may still outweigh the risks. As with any medication, informed decision-making and proper medical oversight are essential.
Frequently Asked Questions
Pancreatitis is inflammation of the pancreas, an organ behind the stomach that helps with digestion and produces insulin. It’s concerning for weight loss drug users because GLP-1 medications like Mounjaro, Wegovy, and Ozempic stimulate the pancreas to produce insulin, which may trigger inflammation in some people. The condition can be serious, requiring hospitalization, and in rare cases (about 5% of acute cases), it can be fatal.
GLP-1 receptor agonist medications including Mounjaro (tirzepatide), Ozempic and Wegovy (semaglutide), and liraglutide products have been linked to pancreas problems. According to MHRA data, Mounjaro has been associated with 181 cases of pancreatitis and five deaths, while Ozempic and Wegovy together have been linked to 113 cases and one death. These medications are used for both diabetes management and weight loss.
Pancreatitis is classified as an “uncommon” side effect of GLP-1 drugs, potentially affecting up to 1 in 100 people. The patient information leaflets for these medications already list pancreatitis as a possible side effect. However, it’s important to note that these reports are based on the MHRA’s Yellow Card scheme, which collects voluntary reports of suspected adverse reactions rather than confirmed causation.
Key symptoms of pancreatitis to watch for include:
- Severe abdominal pain (often radiating to the back)
- Nausea and vomiting
- Fever
- Tender abdomen when touched
If you experience these symptoms while taking GLP-1 medications, seek immediate medical attention and inform healthcare providers about your medication use. Early diagnosis and treatment are important for managing pancreatitis.
Research suggests certain groups may be at higher risk for developing pancreatitis when taking GLP-1 drugs:
- People with a history of type 2 diabetes
- Tobacco users
- Those with advanced chronic kidney disease (stage 3 or higher)
Interestingly, research has found that having a higher BMI (over 36) may actually provide some protection against developing pancreatitis with these medications. The MHRA is currently studying whether genetic factors may also influence susceptibility.
You should not stop taking your prescribed medication without consulting your healthcare provider. While reports of pancreatitis are concerning, for many people with type 2 diabetes or obesity, the benefits of GLP-1 drugs may still outweigh the risks. Every individual’s situation is different.
Healthcare professionals advise:
- Only take these medications under proper medical supervision
- Discuss any history of pancreatitis with your doctor before starting treatment
- Be aware of pancreatitis symptoms and seek immediate medical attention if they develop
- Report any suspected side effects to the appropriate health authorities (like the MHRA’s Yellow Card scheme)
Your doctor can help you evaluate your personal risk factors and make an informed decision.