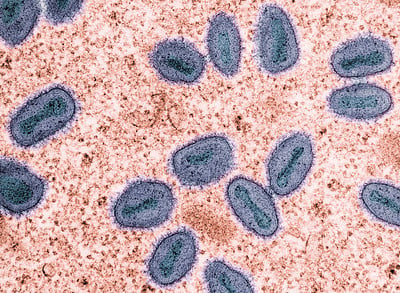
A returned traveler at Logan Hospital has been diagnosed with the more severe Clade I mpox strain, marking only the second such case ever recorded in Australia. Health officials have swiftly identified 59 close contacts, all now isolating, as they work to contain this rare strain. Here’s what you need to know about this case, the virus, and the public health response.
The Case: Fast Facts
The male patient contracted the virus in central Africa before returning to Brisbane. Queensland Health Minister Tim Nicholls confirmed the patient is stable with “relatively mild symptoms” and sought treatment promptly at Logan Hospital’s emergency department.
“Those close contacts that he has been in contact, including at the emergency ward and in other locations, are being contact traced right now and identified at this stage,” said Health Minister Tim Nicholls. He added, “Contact tracing has been occurring, and the community can be assured that exposure to members of the community has been very limited, and the public should not be concerned.”
Health authorities have identified two contact groups:
- 19 community contacts (primarily family members, including children in school and childcare)
- 40 healthcare staff at Logan Hospital
All contacts have received post-exposure vaccination and are under active monitoring. The patient was not contagious during his flight to Australia, significantly limiting potential spread.
What Makes Clade I Different from Regular Mpox?
Clade I (formerly known as the Congo Basin strain) comes with some important differences compared to the more common Clade II strain that caused the 2022 global outbreak:
- Higher fatality rate (up to 10% in endemic regions) compared to Clade II’s less than 1%
- More severe symptoms and complications
- Fever and swollen lymph nodes more pronounced
- Rash typically appears 1-5 days after fever onset
“The contagion window we define as being four days before the onset of symptoms, until after the skin lesions have crusted over,” explained Dr. Geoffrey Playford from Metro South Hospital Service.
Symptoms and Timeline: What to Watch For
The virus has a 5-21 day incubation period (usually 6-16 days). People exposed to someone with mpox should monitor for symptoms for 21 days from their last contact.
The illness typically progresses in stages:
- Early symptoms: Fever, headache, muscle aches, swollen lymph nodes, fatigue
- Rash development: Small bumps appear 1-5 days after fever, often on face, hands, genitals, or perianal areas
- Progression: Bumps fill with fluid, then pus, before crusting over and healing (2-4 weeks total)
Complications can include bacterial infections, pneumonia, and rarely, encephalitis. These are more common with Clade I infections.
Transmission: How It Spreads
Unlike COVID-19, mpox doesn’t spread easily. Transmission requires prolonged close contact through:
- Direct skin-to-skin contact with rash or lesions
- Respiratory droplets during prolonged face-to-face contact
- Touching contaminated items like clothing or bedding
Public health officials stress that casual contact in public settings poses minimal risk.
Global Context: The 2023-2025 Mpox Situation
As of July 2025, fourteen countries in Africa have reported Clade I detections, with Democratic Republic of Congo and Uganda reporting the most cases. According to the CDC, the countries experiencing sustained human-to-human transmission include Burundi, Democratic Republic of the Congo, Ethiopia, Kenya, Malawi, Rwanda, South Sudan, Tanzania, Uganda, and Zambia.
Since August 2024, travel-associated cases of Clade I mpox have been reported in 22 countries outside Africa, including Australia, Belgium, Brazil, Canada, China, France, Germany, India, the United Kingdom, and the United States.
The World Health Organization declared a Public Health Emergency of International Concern on August 14, 2024, for this epidemic.
The global outbreak of Clade II mpox that began in 2022 has caused more than 100,000 cases across 122 countries with over 220 reported deaths.
Vaccine Information: Protection and Eligibility
Queensland offers free mpox vaccines to:
- Close contacts of confirmed cases
- Sexually active gay and bisexual men and their partners
- Travelers to/from outbreak regions
- Laboratory and clinical workers handling the virus
The JYNNEOS vaccine provides significant protection against mpox, with studies showing 66% effectiveness after two doses. According to the New England Journal of Medicine, “Among 2193 case patients and 8319 control patients, 25 case patients and 335 control patients received two doses (full vaccination), among whom the estimated adjusted vaccine effectiveness was 66.0% (95% confidence interval [CI], 47.4 to 78.1).”
For best results after exposure, vaccination should occur within 4 days, though it may help up to 28 days after contact. Common side effects include injection site pain, redness, fatigue, and headache.
Prevention Measures: Practical Steps
For healthcare settings:
- N95/P2 respirators, gowns, gloves, and eye protection
- Environmental disinfection with hypochlorite solutions
- Steam laundry for potentially contaminated linens
For community settings:
- Avoid sharing bedding, towels, or clothing with someone who might be infected
- Practice good hand hygiene
- Disinfect high-touch surfaces
- Consider vaccination if in a high-risk group or traveling to affected regions
Key Takeaways
Queensland Health is managing a rare Clade I mpox case in a returned traveler from central Africa. There have been 135 cases of Clade II mpox in Queensland over the past year, but this is only the second time Clade I has been detected in Australia. The first case was reported in NSW in May 2025.
Close contacts are vaccinated and isolating, with health officials confident about containing the situation. Free vaccines are available for eligible groups through sexual health clinics and GPs.
If you’ve had close contact with someone showing mpox symptoms or are concerned about potential exposure, contact your GP or hospital by phone before visiting in person.
For more information about mpox, visit the Queensland Health website or call 13 HEALTH (13 43 25 84).
Frequently Asked Questions about the Brisbane Mpox Case
What is Clade I mpox and how dangerous is it?
Clade I mpox is a more severe strain of the mpox virus. It has a higher fatality rate (up to 10% in some African regions) compared to the more common Clade II strain (less than 1%). However, with good medical care, most people recover completely. The Brisbane case is only the second Clade I case ever detected in Australia.
How does mpox spread? Should I be worried about catching it?
Mpox doesn’t spread easily in everyday situations. It requires close, prolonged contact like:
- Direct skin-to-skin contact with rashes or lesions
- Prolonged face-to-face contact with someone infected
- Touching items like clothing or bedding used by someone with mpox
Queensland Health officials have stressed that the risk to the general public is very low. Normal daily activities pose virtually no risk.
What are the symptoms I should watch for?
Mpox symptoms typically develop in stages:
- First signs: Fever, headache, muscle aches, swollen lymph nodes, feeling tired
- 1-5 days later: A rash appears, often starting on the face before spreading to other parts of the body
- Over 2-4 weeks: The rash changes from flat spots to raised bumps to fluid-filled blisters that eventually scab over and heal
If you’ve had close contact with someone with mpox and develop these symptoms, call your doctor before visiting in person.
Who is eligible for the mpox vaccine in Queensland?
Free mpox vaccines are available in Queensland for:
- Close contacts of confirmed mpox cases
- Sexually active gay and bisexual men and their partners
- People traveling to/from regions with mpox outbreaks
- Laboratory and healthcare workers who may handle the virus
The vaccine works best when given before exposure but can still help if given within 4 days after exposure.
How effective is the mpox vaccine?
The JYNNEOS vaccine is about 66% effective at preventing mpox after two doses. Even in breakthrough cases, vaccinated people typically experience milder symptoms. The vaccine requires two doses given 28 days apart for maximum protection.
Side effects are usually mild and include pain at the injection site, fatigue, headache, and muscle aches that typically resolve within a few days.
What should I do if I think I’ve been exposed to mpox?
If you think you’ve been exposed to mpox:
- Call your GP or 13 HEALTH (13 43 25 84) for advice
- Mention your potential exposure
- Monitor for symptoms for 21 days
- Avoid close contact with others if you develop symptoms
- If possible, get vaccinated within 4 days of exposure
Always call ahead before visiting a healthcare facility if you suspect you have mpox symptoms.
How long does it take to recover from mpox?
Most people recover completely from mpox within 2-4 weeks without specific treatment. During this time, the rash goes through several stages before healing completely.
A person is considered infectious from about 4 days before symptoms appear until all the scabs have fallen off and fresh skin has formed underneath. This means isolation may be needed for up to a month in some cases.
Test Your Mpox Knowledge
How much do you know about mpox? Take this quick quiz to find out!