Scientists at the University of Surrey have discovered how to target tuberculosis (TB) bacteria that hide from antibiotics. This finding could lead to better treatments for a disease that kills 1.3 million people every year.
TB remains deadly not just because of drug resistance, but because some bacteria can survive treatment by becoming dormant – earning them the nickname “zombie cells.” These cells essentially play dead during antibiotic treatment, then reawaken once treatment stops, causing infection to return.
“Tuberculosis really is the forgotten pandemic,” says Dr. Suzie Hingley-Wilson from the University of Surrey. “It killed 1.3 million people last year, mostly from completely drug-sensitive strains. The problem isn’t always resistance—it’s persisters.”
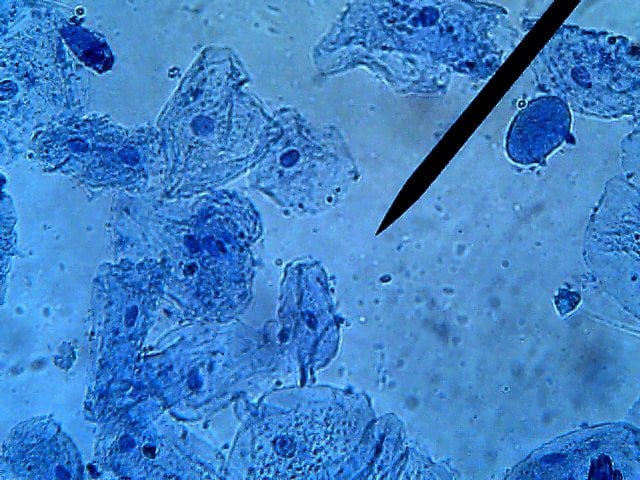
The Surrey research team exposed over 500,000 genetically modified TB bacteria to common antibiotics – rifampicin and streptomycin. By studying which bacteria survived, they identified specific genes that help these zombie cells stay alive during treatment.
Their key discovery challenges what scientists previously believed. Rather than using the same survival tactics against all antibiotics, TB bacteria use different genetic pathways depending on which drug they face.
“What we found is that persister survival depends on the antibiotic used,” explains Dr. Hingley-Wilson. “The mechanisms aren’t shared as previously thought; they’re drug-specific.”
The researchers found these critical genes perform various roles: some strengthen the bacterial cell wall, others prevent bacterial self-destruction, and some maintain the cell’s metabolism. When these genes were disrupted, far fewer bacteria survived antibiotic treatment.
Professor Johnjoe McFadden, who led the study, believes this could transform how we treat TB. “The mechanisms involved in persistence are probably the biggest mysteries in microbiology. Their solution could revolutionize treatment.”
Similar Post
Current TB treatment requires months of multiple antibiotics. Many patients struggle to complete such long treatments, which contributes to the rise of drug resistance. If new drugs could target these persistence mechanisms, treatment times could potentially be shortened dramatically.
The World Health Organization has identified antimicrobial resistance as one of the top 10 global health threats. Finding new ways to kill bacteria becomes increasingly urgent as more bacteria evolve to resist our current antibiotics.
This research represents a shift from previous approaches. While scientists have long focused on bacterial resistance – genetic mutations that allow bacteria to disable antibiotics – persisters don’t mutate. They temporarily enter a dormant state that antibiotics can’t affect.
The next research phase will focus on developing new drugs that mimic these gene functions. This could lead to treatments that specifically target and eliminate TB persister cells, potentially saving millions of lives.
For patients, this breakthrough could mean shorter treatments – possibly weeks instead of months – making TB treatment more manageable and effective. This could significantly reduce TB’s global impact and slow the spread of antimicrobial resistance.
While developing approved treatments will take time, this discovery provides a clear direction for TB drug development. By targeting the genetic weaknesses of persister cells, future treatments may finally overcome one of TB’s most effective survival strategies.
The research offers new hope for effective treatments against a disease that has plagued humanity for centuries. By understanding how to eliminate even the most stubborn TB cells, scientists are one step closer to controlling this deadly infection.
The research was published in Scientific Reports and marks a significant advance in fighting one of the world’s most dangerous infectious diseases.
Frequently Asked Questions
“Zombie” TB cells (scientifically known as persister cells) are tuberculosis bacteria that enter a dormant state when exposed to antibiotics. Unlike resistant bacteria that have genetic mutations, these cells “play dead” during treatment by slowing their metabolism. Once antibiotics are removed, they reactivate and restart the infection. This is why TB treatment requires months of antibiotics and still often fails, contributing to 1.3 million deaths annually worldwide.
University of Surrey scientists discovered that TB bacteria use different genetic pathways to survive different antibiotics – a phenomenon called “drug-specific persistence.” By testing 500,000 genetically modified TB bacteria, they identified specific genes that help these zombie cells survive. The research team pinpointed genes responsible for strengthening cell walls, preventing cellular self-destruction, and maintaining metabolic balance – all potential targets for new drugs.
Previous TB research primarily focused on bacterial resistance – genetic mutations that allow bacteria to disable antibiotics. This new approach targets persistence mechanisms instead. Scientists previously believed all persisters used the same survival tactics against different antibiotics, but this research proves that survival is drug-specific. This discovery changes how scientists think about targeting persisters and could reshape how future TB treatments are designed.
Current TB treatment requires months of multiple antibiotics, which many patients struggle to complete. By developing drugs that specifically target the genetic pathways that enable zombie cells to survive, treatments could potentially be shortened from months to weeks. This would improve patient adherence, reduce the global burden of TB, and slow the rise of antimicrobial resistance.
Despite killing 1.3 million people annually (more than many high-profile diseases), TB receives relatively little public attention and research funding. Dr. Hingley-Wilson from the University of Surrey calls it “the forgotten pandemic” because most deaths come from completely drug-sensitive strains – the problem isn’t always resistance but persisters. TB primarily affects lower-income countries, which may contribute to its lower profile despite its massive global health impact.
The next phase of research will focus on developing novel therapeutics that mimic the gene functions identified in the study. Scientists will work to create drugs that can specifically target and eliminate TB persister cells by disrupting the genetic pathways that help them survive. While the path from laboratory discovery to approved treatments is long, this breakthrough provides a clear direction for TB drug development that could potentially save millions of lives globally.