Scientists at the University of Copenhagen have discovered that bacteria from cows might offer a powerful new way to treat dangerous MRSA infections. Their research shows that these bacteria can disrupt MRSA’s ability to cause infection as effectively as traditional antibiotics.
MRSA (methicillin-resistant Staphylococcus aureus) infections are increasingly difficult to treat because they resist common antibiotics. This discovery could provide a much-needed alternative in the global fight against antibiotic resistance.
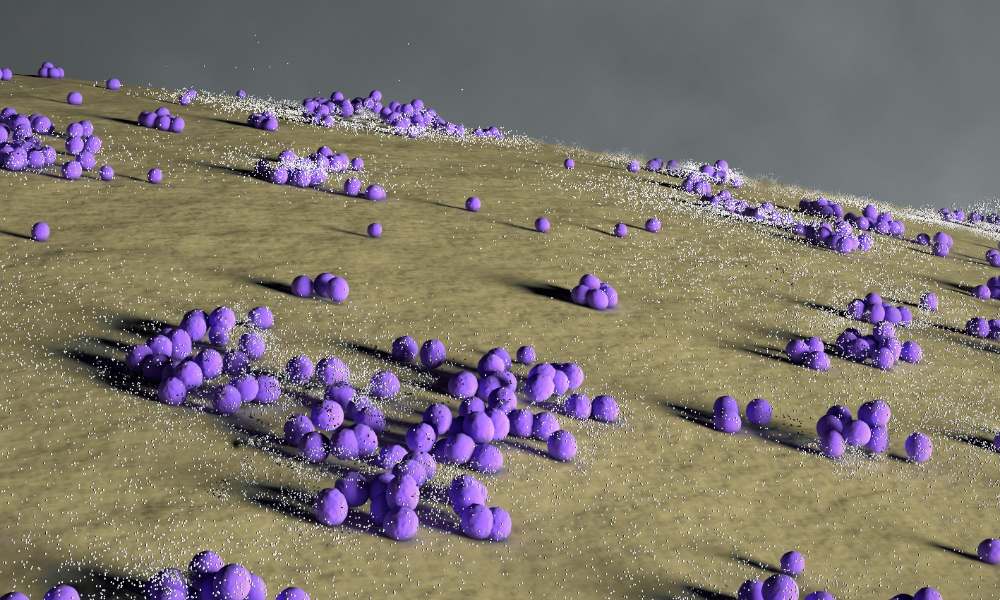
The Danish researchers focused on how bacteria “talk” to each other using chemical signals. Professor Christian Adam Olsen, who led the study, explained this communication using a simple comparison: “Imagine two people talking over a walkie-talkie set. Successful communication depends on them being tuned to the same frequency.”
When bacteria like MRSA infect a wound, they use these signals to coordinate their attack. The researchers found that signals from a different bacteria called Staphylococcus simulans can effectively jam MRSA’s communication.
“We found that a signal from Staphylococcus simulans was very potent against S. aureus,” said Professor Olsen. “Originally, the signaling molecule was isolated from a bacterial strain from a cow, but it is also present on goats, horses and humans.”
In laboratory tests with mice, the results were remarkable. A single dose of the S. simulans signal molecule cleared MRSA skin infections as effectively as daily applications of antibiotic ointment.
Postdoc Benjamin Svejdal Sereika-Bejder, who worked on the study, noted: “With a single dose of this signaling molecule, the mice could overcome an MRSA skin infection just as effectively as mice treated daily with an antibiotic ointment.”
What makes this approach particularly promising is that it doesn’t kill bacteria outright. Instead, it prevents them from communicating effectively, which weakens their ability to cause infection. This difference is crucial because it might help avoid the problem of antibiotic resistance.
“In our experiments, we observed that under laboratory conditions, the bacteria did not develop resistance even after 15 days,” said Sereika-Bejder. “This is very promising but will require further testing in animal models.”
The researchers conducted the most extensive mapping to date of these bacterial signaling molecules. They identified 35 different signals across 21 species of Staphylococcus bacteria and documented 280 interactions between them. This comprehensive mapping helped them pinpoint which signals would be most effective against MRSA.
Similar Posts
Professor Olsen explained why bacteria might not develop resistance to this treatment: “There is likely no evolutionary pressure on the bacteria to develop resistance, as they don’t perceive the signaling molecules as being lethal to them. They are also encountering these signaling molecules from other bacteria in their natural environment.”
The global impact could be significant. Bacterial antimicrobial resistance directly caused 1.27 million deaths worldwide in 2019, with MRSA being a major contributor to this toll.
The research highlights the value of exploring livestock microbiota in the “One Health” approach, which recognizes the connections between human, animal, and environmental health.
The study was published in July 2025 in the scientific journal mBio, and researchers are now advancing to larger animal trials. If successful, this cow-derived bacterial signal could eventually provide doctors with a powerful new tool against dangerous MRSA infections that resist conventional antibiotics.
Frequently Asked Questions
MRSA (Methicillin-Resistant Staphylococcus aureus) is a type of bacteria that has developed resistance to many common antibiotics, including methicillin. It’s dangerous because infections caused by MRSA are difficult to treat with standard antibiotics, can spread rapidly, and may lead to serious health complications. MRSA infections range from skin infections to more severe conditions like pneumonia or bloodstream infections. In 2019, bacterial antimicrobial resistance directly caused 1.27 million deaths worldwide, with MRSA being a significant contributor.
The treatment uses signaling molecules from Staphylococcus simulans, a bacteria originally isolated from cows. Rather than killing MRSA bacteria directly, these molecules disrupt their communication system (called quorum sensing). Think of it like jamming a walkie-talkie frequency – the MRSA bacteria can no longer coordinate their attack on the body. This communication disruption weakens their ability to cause infection, allowing the body’s immune system to fight back more effectively.
No, this treatment is not yet available for humans. So far, the research has only been conducted in laboratory settings and on mice. The University of Copenhagen researchers are now advancing to larger animal trials. If these trials are successful, the treatment would still need to go through human clinical trials and regulatory approval before becoming available as a medical treatment. This entire process typically takes several years.
This discovery is significant for three main reasons: First, it requires only a single dose to be as effective as daily antibiotic treatments, which could improve patient compliance and reduce healthcare costs. Second, after 15 days of continuous exposure in laboratory tests, MRSA showed no signs of developing resistance to this treatment, whereas resistance to antibiotics is a growing global crisis. Finally, because it doesn’t kill bacteria but instead disrupts their communication, there’s less evolutionary pressure for the bacteria to develop resistance, potentially offering a more sustainable long-term solution.
While the current research specifically focused on MRSA, there’s potential for similar approaches to work against other bacteria. The researchers mapped 35 different signaling molecules across 21 staphylococcal species, revealing 280 pairwise interactions. This extensive mapping suggests that bacterial communication disruption could potentially be applied to other bacterial species that use similar quorum sensing systems. However, more research would be needed to confirm effectiveness against other types of antibiotic-resistant bacteria.
The research is still in early stages, so comprehensive information about potential side effects in humans isn’t available yet. One potential advantage of this approach is that it doesn’t kill the bacteria but rather disrupts their communication, which might result in fewer side effects than traditional antibiotics that can disrupt beneficial bacteria in the gut and elsewhere in the body. However, thorough safety testing will be required during animal and human trials to identify any possible risks or side effects before the treatment could be approved for clinical use.