Cancer remains one of the world’s deadliest health challenges, with 9.7 million deaths globally in 2022. For Americans, the outlook is equally concerning—over 2 million new cancer cases and more than 600,000 deaths are projected for 2025. But scientists are making progress on a promising front: detecting cancer earlier through breath analysis.
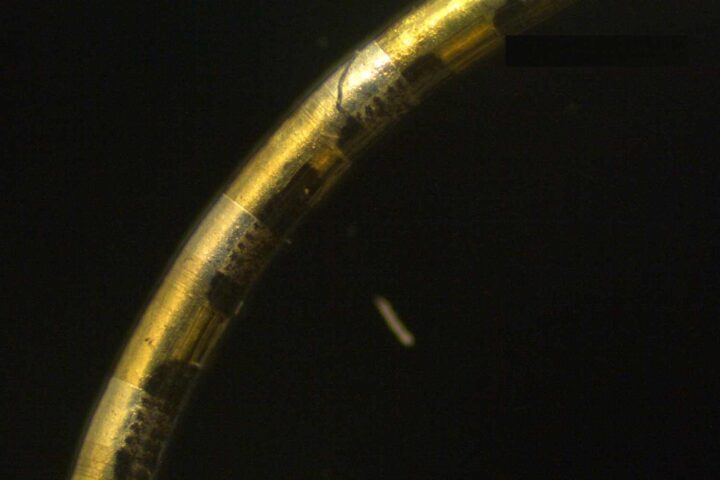
At Binghamton University, chemistry professor Chuan-Jian “CJ” Zhong didn’t set out to revolutionize cancer screening. His team initially developed tiny sensors to detect harmful gases in fighter jet cockpits. An unexpected shift led them to apply this technology to healthcare.
“We thought, ‘Hey, since we have been working this sensor for a long time now, we should also do that,'” Zhong explains.
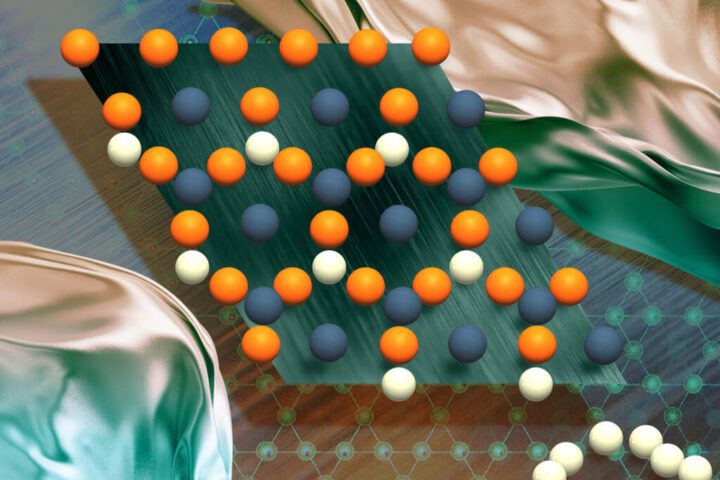
The technology works by capturing chemical compounds in breath that may signal cancer. When a patient breathes into the device, these compounds pass over special sensors. If cancer markers are present, they create electrical signals that can be analyzed.
Similar Posts
To make sense of this data, Zhong works with systems science professor Susan Lu, whose expertise in pattern recognition and artificial intelligence helps interpret the signals. Their combined approach creates a potential screening method that could add to traditional diagnostics.
Current cancer detection often involves invasive procedures. For lung cancer—a particularly deadly form where about 27% of cases are caught early—patients typically undergo CT scans or painful tissue biopsies. More than half of people diagnosed with lung cancer die within a year, highlighting the urgent need for earlier detection tools.
Zhong sees two futures for this technology: placing breath analyzers in doctors’ offices for routine screening, and developing smaller sensors that could connect to smartphones for regular at-home checks.
“Right now, cancer screening is a CT scan, a blood test or other methods that are time-consuming and sometimes even invasive,” he says. “We want to take a breath sample and diagnose: cancer or no cancer. This gives a patient an early warning to go to a doctor to double-check.”
The research faces practical challenges. Collecting enough breath samples from cancer patients is difficult since “it’s not like everybody’s coming to the doctor at the same time,” as Zhong notes. His team gathers samples from Cooper University Hospital in New Jersey and a partner hospital in China.
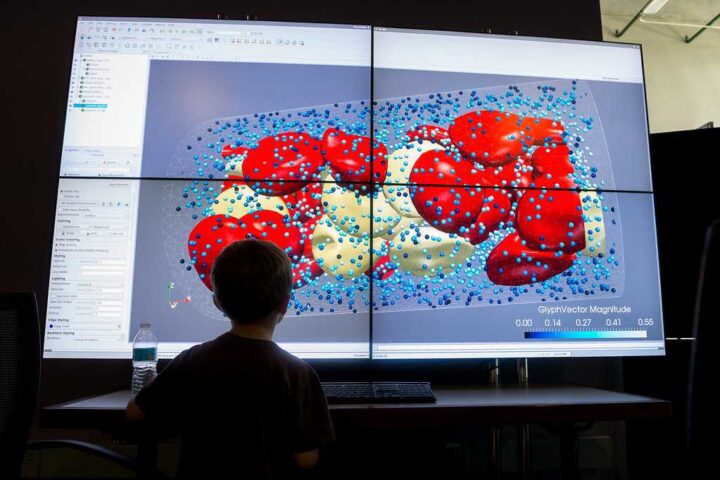
Other cancer detection innovations at Binghamton include Yuan Wan’s blood-based approach for analyzing tiny cellular components. His method can diagnose cancerous lung nodules with over 90% accuracy when combined with AI analysis of CT scans.
Biomedical engineer Frank Lu is developing laser technology that tells cancer cells from healthy ones by analyzing how they scatter light differently. His approach could help surgeons identify cancer cells during operations.
Meanwhile, computing professor Nancy Guo believes untapped potential exists in genetic data already being collected. Her team developed a genetic test for lung cancer that shows about 95% accuracy for predicting whether tumors will return or spread.
While these technologies show promise, they still require extensive testing through clinical trials. Questions remain about how they compare to standard screenings, regulatory approval, and integration into healthcare systems.
For patients, the stakes couldn’t be higher—earlier, less invasive detection could transform cancer from a deadly diagnosis to a manageable condition.