Scientists at MIT and Harvard Medical School have developed a new type of cancer-fighting cell that could transform how we treat cancer. These cells, called CAR-NK cells, have been engineered to hide from a patient’s immune system while being more effective at killing cancer.
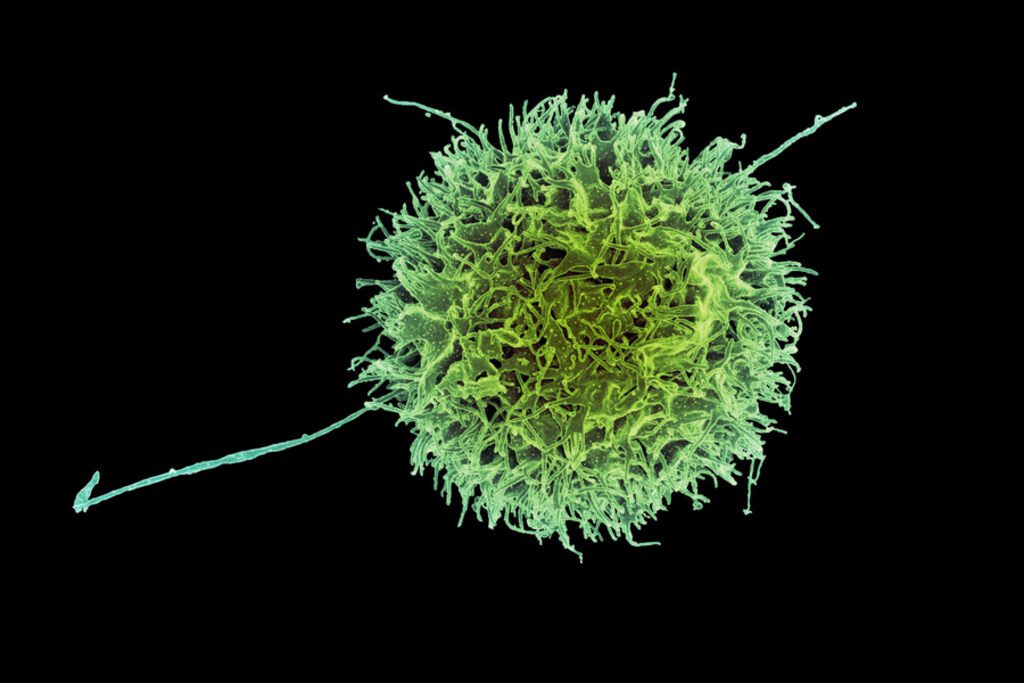
Natural killer (NK) cells are part of our body’s immune system that naturally hunt and destroy cancer cells. Scientists can enhance these cells by adding a special protein called a chimeric antigen receptor (CAR), which helps them target cancer more precisely.
The main breakthrough came when researchers found a way to make these cells invisible to the patient’s immune system. “This enables us to do one-step engineering of CAR-NK cells that can avoid rejection by host T cells and other immune cells. And, they kill cancer cells better and they’re safer,” explains Jianzhu Chen, an MIT professor and member of the Koch Institute for Integrative Cancer Research.
Similar Posts
In traditional cell therapies, doctors must take cells from a patient, modify them in a lab, and then return them to the patient—a process that can take weeks. The new technique could allow “off-the-shelf” treatments using cells from healthy donors that are ready whenever needed.
The engineering involved three key modifications: adding the cancer-targeting CAR, using siRNA to suppress HLA class I proteins (which normally trigger immune rejection), and adding either PD-L1 or single-chain HLA-E proteins to boost the cells’ cancer-killing ability.
When tested in mice with human-like immune systems and lymphoma, these modified NK cells lasted at least three weeks in the body and nearly eliminated cancer. In contrast, NK cells without these modifications were destroyed by the immune system within two weeks, allowing cancer to spread unchecked.
An added benefit is that these engineered cells were less likely to cause cytokine release syndrome, a potentially dangerous side effect of some cancer immunotherapies.
The research team, which includes senior authors Chen and Rizwan Romee of Harvard Medical School and Dana-Farber Cancer Institute, along with lead author Fuguo Liu, is now planning clinical trials. They’re also exploring using similar cells to treat lupus, an autoimmune disorder.
This research was published in Nature Communications and received funding from Skyline Therapeutics, the Koch Institute Frontier Research Program, the Claudia Adams Barr Foundation, and the National Cancer Institute.