Scientists are making major progress in fighting Parkinson’s disease with new discoveries about early detection and environmental risks. These advances could change how doctors diagnose and possibly prevent this brain disorder that affects nearly one million Americans.
New AI technology is helping doctors identify Parkinson’s disease earlier and more accurately. Research shows this technology can tell Parkinson’s apart from similar conditions with impressive results.
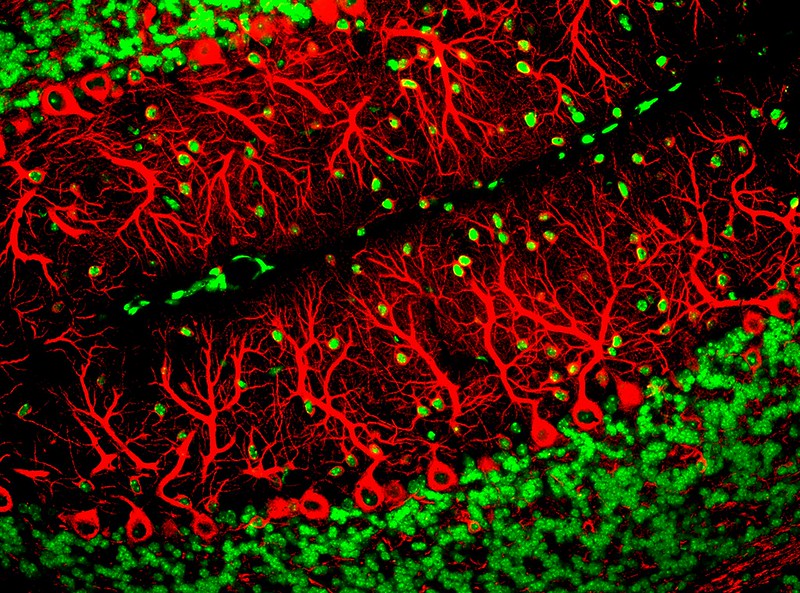
The technology works by analyzing brain MRI scans. Scientists studied 249 patients across 21 medical centers in the U.S. and Canada. The AI system learned to spot tiny differences between Parkinson’s disease and two similar conditions that are often confused with it.
The results were striking – the AI approach correctly identified Parkinson’s 96 percent of the time when comparing it to similar movement disorders. It was even more accurate – 98 percent – when distinguishing between specific conditions. Most impressive was that the AI correctly predicted what would be found in brain tissue after death in 94 percent of cases, while traditional clinical diagnosis was right only 81.6 percent of the time.
Dr. Rizwan Akhtar from Northwestern University explained why this matters: “It can be hard to confirm these diagnoses early on. If a person has one of these disorders, we want to identify that as soon as we can to counsel the family and patient about what to expect.”
This technology could help more people get the right diagnosis without traveling to specialized medical centers. An MRI can be done at many hospitals and the results could be analyzed using this AI system.
While doctors work on better diagnosis, researchers are also finding stronger evidence linking certain pesticides to Parkinson’s risk.
A large study looked at data from over 21.5 million older adults and pesticide use across rural counties in the Rocky Mountain and Great Plains region between 1992 and 2008. They found that 14 pesticides were strongly connected to higher Parkinson’s disease risk.
Three pesticides showed the strongest connection to Parkinson’s:
Simazine (a weed killer): 36% higher risk Lindane (a banned insect killer): 25% higher risk Atrazine (another weed killer): 31% higher risk
Similar Posts:
People living in areas with the highest use of these chemicals were much more likely to develop Parkinson’s compared to those in areas with the lowest use. The study found that more pesticide use in a county meant greater Parkinson’s risk among residents.
This isn’t the first time pesticides have been linked to Parkinson’s. Scientists have suspected connections between chemical exposure and Parkinson’s since the 1980s. A 2011 study also found links between different pesticides and increased Parkinson’s risk.
What’s concerning is that the U.S. allows many pesticides that other countries have banned. In 2016, U.S. agriculture used about 1.2 billion pounds of pesticides. Of that amount, 322 million pounds were banned in the European Union, 40 million pounds were banned in China, and nearly 26 million pounds were banned in Brazil.
Dr. Brittany Krzyzanowski, who led the pesticide study, pointed out: “It’s concerning that previous studies have identified other pesticides as potential risk factors for Parkinson’s, and hundreds of pesticides have not yet been studied for any relationship to the disease.”
Parkinson’s affects nearly one million Americans, with about 90,000 new cases each year. The disease causes tremors, muscle stiffness, and slowed movement. It also brings non-motor symptoms like depression and thinking problems.

These new research directions offer hope. The AI imaging approach could help doctors diagnose patients sooner and get them appropriate treatments earlier. Better understanding of pesticide risks could lead to stronger regulations and prevention strategies.
While pesticides are still needed for farming, these findings show we need more research into their long-term health effects and safer alternatives.