A University of Houston scientist has developed a groundbreaking approach to treat lupus by delivering medication directly to the spleen, potentially offering patients a more effective treatment with fewer side effects.
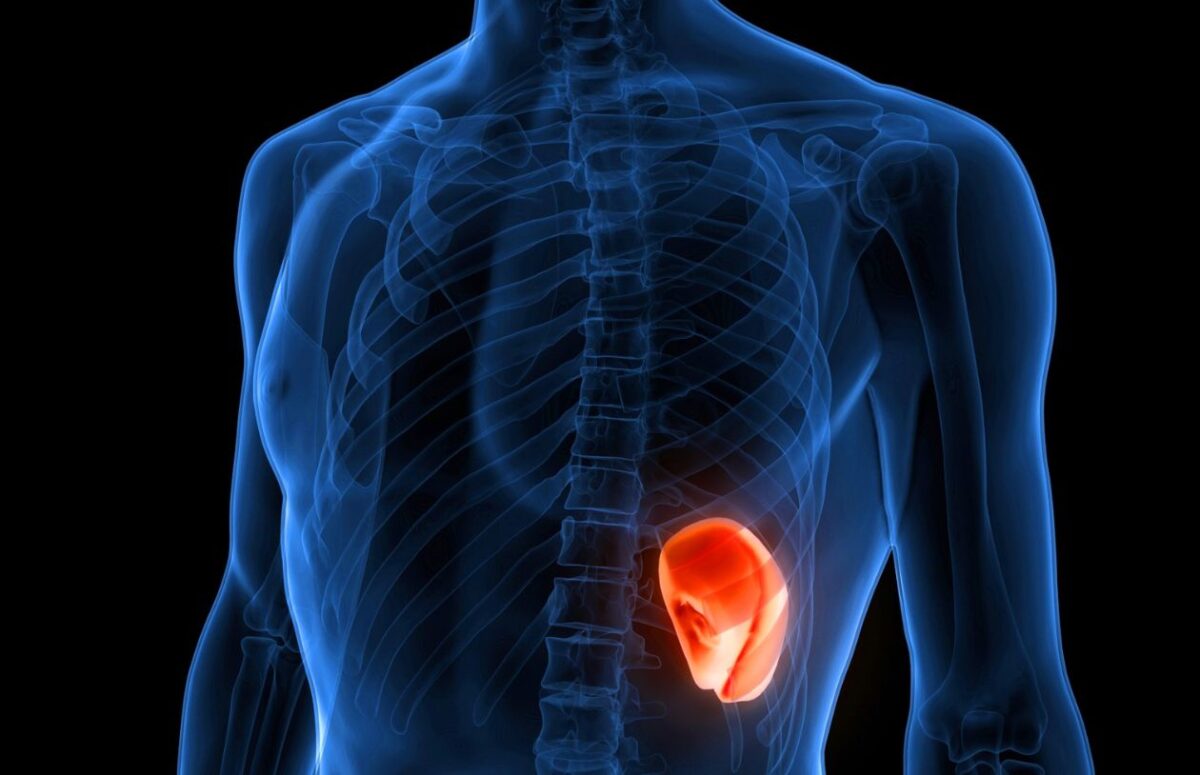
Biomedical engineer Tianfu Wu received a $1 million Impact Award from the U.S. Department of Defense to create what may be the first spleen-specific drug delivery system for lupus. The innovative approach uses tiny fat-based particles, called lipid nanoparticles, modified with mannose (a simple sugar) to deliver medicine directly to immune cells in the spleen that drive lupus.
“The current therapeutic landscape for lupus is often marred by systemic side effects and relatively limited efficacy,” said Wu, an associate professor of biomedical engineering. “We are proposing a spleen-specific selective organ targeting lipid nanoparticle drug delivery system to modulate immune responses and mitigate symptoms with minimal side effects.”
The disease disproportionately affects women, particularly those of childbearing age, with 9 out of 10 lupus patients being female. Black, Hispanic, Asian, and Native American populations are also more likely to develop the condition than white populations.
Similar Posts
The spleen plays a critical role in lupus as it houses millions of immune cells that contribute to the disease. Wu’s system targets B cells, plasmacytoid dendritic cells, and macrophages – key immune cells that drive lupus inflammation.
Current lupus treatments often rely on broad immunosuppression or B-cell depletion. These approaches can cause severe side effects, increase infection risks, and may eliminate beneficial immune cells. Common treatments include antimalarials like hydroxychloroquine, corticosteroids like prednisone, and immunosuppressants that affect the entire immune system.
Wu’s research recognizes that the same drug target may have different roles in different organs. “This innovation will pave the way for treating lupus by targeting organ-specific molecular pathways,” he explained. “The same drug target may have opposing roles in different organs, such as the spleen versus the kidney, heart, or central nervous system.”
If successful, this targeted approach could offer lupus patients a treatment that specifically addresses disease activity where it begins rather than suppressing the entire immune system. This precision could potentially reduce side effects while improving symptom control for a disease that currently has no cure.
The spleen-targeted approach represents a significant shift from conventional therapies, offering hope for improved quality of life for those living with this challenging autoimmune condition.